Vein pathologies in women are a common phenomenon. Gender is determined by hormonal changes, lifestyle characteristics, body functionality and other factors. Veins can be damaged under the influence of external and internal factors. This leads to stretching of the blood vessels, thinning of the walls, formation of plaques, dysfunction of the valves, thickening of the blood and other negative consequences. Varicose veins of the small pelvis in women is a type of vein pathology. It is characterized by discomfort, pain, a feeling of heaviness and pressure, and sometimes even leads to dysfunction of the reproductive system.
What are varicose veins of the small pelvis
Fleberismis a pathology characterized by a change in the normal state of the vessels and veins of the human body. ICD-10 does not have a separate classification. Diseases of the veins are indicated by code I80-I89. A separate classification includes varicose veins of the lower extremities (I83. 9), which are often combined with varicose veins of the small pelvis in women.
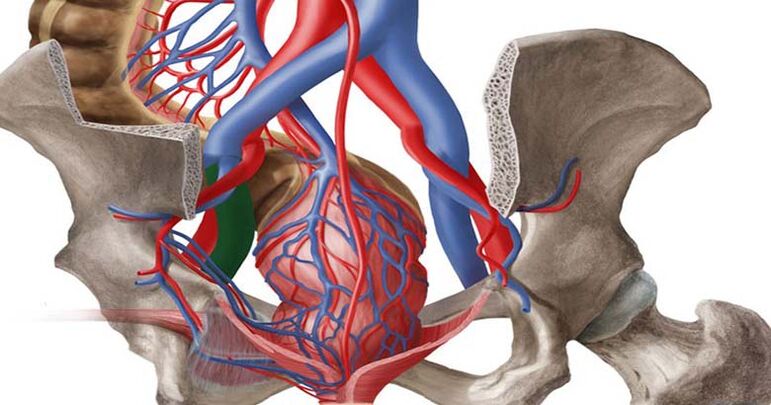
With varicose veins of the small pelvis, there is thinning of the walls of the blood vessels, their expansion and stretching. In this state, the blood stagnates. Due to the decrease in tone, the vessels cannot fully function and pump blood, as a result of which peculiar knots are formed in them, which are popularly called varicose veins.
In recent years, there has been a trend towards a rejuvenation of the disease. If previously varicose veins of the small pelvis mainly affected elderly women, now the pathology is more and more common in young patients. According to statistics, up to 20% of women of childbearing age have varying degrees of varicose veins. Varicose veins of the pelvis (PVVD) are often accompanied by other pathological processes, which seriously complicates the diagnostic procedure.
Varicose veins affect the function of the pelvic organs. It can be accompanied by severe symptoms or no clinical manifestations. In difficult situations, it becomes a cause of complications. The treatment of varicose veins is chosen individually and does not always achieve the desired result.
Classification of varicose veins of the small pelvis
Varicose veins in the pelvis appear differently in different women. Some patients complain of severe symptoms, while others practically do not experience manifestations of pathology. For some, even serious treatment does not allow them to completely get rid of the pathology, while others can easily cope with the disease through lifestyle changes. In gynecology, a classification of varicose veins of the small pelvis is accepted, which accurately characterizes the development of the pathology.
Forms of varicose veins of the small pelvis
Varicose veins of the pelvis in women are accompanied by a decrease in the tone of the vascular wall, weakening, reduced elasticity and the formation of ectasia - an increase in the lumen in a limited area of the vein.
There are two forms of pelvic varicose veins:
- Varicose veins of the vagina and external genitalia (perineum)- characterized by a change in the structure of the channels of the large vein, as a result of which the external genital vein is affected. Often the cause is a long-term pregnancy, during which compression of the inferior vena cava and iliac vein occurs from the enlarged uterus.
- Venous stasis syndrome- characterized by dilation and stretching of the veins inside the pelvis and the return of blood through them. The causes of such reflux can be very different.
Stages of varicose veins of the small pelvis
Varicose veins of the pelvic organs can occur in three stages. As the disease progresses, one stage replaces another. The stages of the disease differ in the severity of the symptoms and the severity of the disease.
- First stage
It is characterized by dilation of the veins up to a diameter of 5 mm. Vascular tone decreases and the network acquires a curved appearance.
- Second stage
It is characterized by a decrease in the elasticity of the vascular bed in the pelvis. The diameter of varicose veins is from 6 to 10 mm. The parametrial vessels and ovarian plexuses are affected.
- Third stage
It is characterized by complete damage to the vascular fibers. The diameter of the expansion exceeds 10 mm. Against the background of progressive varicose veins, a woman can develop complications.
Character of development
According to the nature of origin and development, varicose veins of the small pelvis are classified:
- Primary varicose veins of the pelvic veins in women
It is formed against the background of acquired or congenital valvular pathologies. Doctors usually talk about valvular insufficiency of the veins, which is accompanied by the appearance of distorted and overstretched vessels. Often, the causes of primary varicose veins are increased physical activity, complications during pregnancy and childbirth, the use of hormonal drugs.
- Secondary varicose veins of the pelvic veins in women
It is formed against the background of past diseases. Infectious pathologies, tumor processes, pelvic endometriosis and abnormal development of the pelvic organs can affect the tone of the veins.
Reasons for the development of varicose veins of the small pelvis
Pathologies of the veins of the pelvic organs can develop due to the following reasons:
- Heredity. Often, vein diseases in women are hereditary. If a mother, grandmother or aunt in the family had varicose veins, then the disease is likely to affect the next female generation.
- Dysplasia of the connective tissue of the pelvic organs. This is a congenital anomaly and is characterized by a decrease in collagen production, against the background of which the tone of the vascular pattern decreases.
- Pregnancy. During pregnancy, the load on muscles and blood vessels increases significantly. The growing uterus puts pressure on adjacent tissues and adjacent veins. With polyhydramnios, multiple pregnancy, large fetus and other conditions, a woman can develop varicose veins.
- Excess body weight. With obesity in women, the pressure on the pelvic organs increases. This can lead not only to the development of varicose veins, but also to other health problems.
- Decreased physical activity. The human body needs regular physical activity. We're not talking about grueling workouts. On the contrary, excessive physical activity can become an independent cause of varicose veins of the small pelvis. With a sedentary lifestyle, blood flow in the pelvis is disturbed and stagnant processes develop.
- Hormonal disorders. The work of the entire female body is completely subordinated to the hormonal levels. Hormonal changes and taking hormonal drugs can cause a decrease in vascular tone.
Varicose veins of the lower extremities are often accompanied by varicose veins of the small pelvis. If a woman has curved vessels on her legs, she should definitely undergo a pelvic examination and, if necessary, undergo treatment.
Risk factors
The risk of developing varicose veins of the small pelvis in women increases with the following factors:
- bad habits;
- tendency to overeat;
- disturbance of the gastrointestinal tract and tendency to constipation;
- lack of intimate life;
- difficult pregnancy;
- surgical interventions;
- pelvic organ injuries;
- hormonal treatment;
- heavy physical exertion.
Symptoms of varicose veins of the pelvic organs
Many women have no symptoms of pelvic varicose veins. The disease can exist for a long time without clinical manifestations. At the same time, the pathology is insidious in that it progresses imperceptibly, which leads to serious health problems.
Signs of varicose veins of the small pelvis in women can be similar to other gynecological pathologies. Therefore, when choosing treatment tactics, it is necessary to carry out a differential diagnosis and exclude other diseases of the pelvic organs.
Common symptoms of varicose veins of the small pelvis:
- pain in the lower abdomen;
- sudden abnormal uterine bleeding;
- discharge unrelated to the menstrual cycle;
- a feeling of bloating and the presence of a foreign body in the pelvis;
- lumbago in the sacrum, lower back, legs, perineum;
- severe premenstrual syndrome;
- severe pain during menstrual bleeding;
- discomfort and pain during intimacy;
- frequent urination;
- dysfunction of the digestive tract.
A characteristic sign of varicose veins in the pelvis in women is the formation of curved bluish veins in the area of the external genital organs and in the vagina.
Diagnosis of varicose veins in the pelvis
Based on the patient's complaints and clinical examination, a preliminary diagnosis can be made. Visually, varicose veins look like cyanotic nodes and dilated vessels. Since the signs of pathology are often confused with other gynecological diseases, to clarify the diagnosis, it is necessary to carry out diagnostics:
- visual examination of the external genitalia;
- examination of the vagina and cervix in speculums;
- palpation and diagnostics of the functionality of the valves in the groin area;
- Ultrasound of the pelvic organs;
- Doppler examination;
- CT;
- magnetic tomography;
- hysteroscopy;
- laparoscopy.
Treatment of varicose veins of the small pelvis
Treatment of pelvic varicose veins in women can be surgical, conservative or complex. The method of treatment is selected individually, in accordance with the clinical manifestations, the stage of varicose veins, the cause of the development of venous pathology and other factors. The main goal of treatment is to reduce the symptoms of the disease and improve the quality of life.
Medicinal treatment of varicose veins of the small pelvis
For varicose veins of the small pelvis, the doctor chooses an individual scheme of drug treatment. The following drugs are traditionally prescribed:
- Venotonics. Modern pharmacology offers many types of venotonics. The main task of the drugs is to increase the elasticity of the blood vessels, normalize the blood flow and stabilize the functioning of the valves. Medicines can be used both for internal use and in the form of ointments.
- Anticoagulants. Medicines are prescribed to thicken the blood due to varicose veins of the pelvis. This parameter is determined by laboratory tests. Blood thinners prevent the formation of blood clots and reduce blood density.
- Nonsteroidal anti-inflammatory drugs. Medicines are used for severe pain and as an additional means of treating the inflammatory process. As a rule, NSAIDs have a symptomatic effect. They relieve the signs of varicose veins of the small pelvis, but do not completely solve the problem.
- Vitamin complexes and trace elements. Since most people are deficient in nutrients and do not get enough from food, supplemental vitamin intake is recommended. For varicose veins, it is recommended to take vitamins B, C, D.
surgery
If drug treatment fails, it is recommended to consider surgical treatment of pelvic varicose veins. The operation is also performed in severe forms of varicose veins.
A modern method of treating varicose veins is endovascular embolization of the gonadal vessels. The procedure is performed in a hospital under general anesthesia. The operation involves inserting coils that block the channel using a catheter into the dilated vein. As a result, the blood flow completely stops in the pathological area. It should be noted that the operation is safe from the point of view of damage to the circulatory system. Since varicose veins themselves are pathological and can no longer function properly, it is advisable to exclude them from the general circulation. Refusal of treatment is accompanied by an increased risk of blood clots in the vessels.
The procedure for endovascular embolization allows solving the problem of varicose veins of the small pelvis in 95% of cases. In the future, the woman is recommended to undergo the prevention of vascular diseases throughout her life.
General recommendations for women with pelvic varicose veins
At each stage of the treatment of varicose veins, as well as after the completion of the correction technique, doctors recommend that women wear compression clothing. After the operation, the period of use of such a leotard is determined individually. Usually, in the first days after the operation, the stockings are worn around the clock. In the future, it is permissible to remove the compression during sleep.
Women with varicose veins of the pelvis are not recommended to engage in heavy sports or carry weights. Baths, saunas and hot baths should be avoided completely. Thermal procedures can worsen the course of varicose veins.
With varicose veins, special attention should be paid to body weight. Excess weight can become a stimulator of varicose veins. That is why it is important to stabilize your body weight and lead an active lifestyle.
Why are varicose veins of the small pelvis dangerous for women?
Complications of varicose veins:
- thromboembolism;
- thrombophlebitis;
- venous thrombosis;
- hemorrhoids;
- hormonal imbalance;
- abnormal uterine bleeding;
- chronic pelvic pain;
- infertility.
Pregnancy and varicose veins of the small pelvis
Varicose veins are not usually a cause of infertility. Varicose and varicose veins can be an increased risk factor for women planning to conceive. It is impossible to say immediately how the body of the expectant mother will behave. The uterus is the main organ for the unborn child. If the blood circulation in the reproductive organ is disturbed or the blood circulation of the placenta is obstructed, then there is a high risk of miscarriage or the formation of various intrauterine disorders.
Prevention of varicose veins of the small pelvis
There is no specific prevention of varicose veins of the small pelvis. Every woman is at risk of developing varicose veins. That's why everyone should follow simple rules:
- healthy life style;
- good nutrition;
- obesity prevention;
- giving up bad habits;
- moderate physical activity;
- drinking enough liquid;
- refusal to wear high heels for a long time;
- rational approach to pregnancy planning and prevention of pregnancy complications;
- the use of compression clothing with a high risk of varicose veins;
- regular scheduled medical examinations.
If varicose veins of the small pelvis have already been found, then the doctor will give recommendations on how to prevent the progression of the disease. As a rule, the woman is prescribed a course of venotonics and regular wearing of compression clothing.


















